Tourette’s syndrome and TMJ
How effective is orthodontics in treating the symptoms of Tourette’s syndrome? André Hedger describes the case of a patient who developed significant ‘tics’ following a seizure
Tourette’s syndrome is characterised by certain tics or abnormal muscle movements and twitches. Various unusual tics display, often in the shoulders or abdomen, as well as eye tics such as chronic blinking or slow blinking and vocal tics such as coughing, humming, barking or swearing.
The condition starts before patients are 18 years old and the tics are not related to any substance or medical condition. Tics can occur multiple times a day and it is not unusual for multiple motor and vocal tics to be present.
Common signs include:
- Eye movement
- Facial grimacing
- Head jerking movement
- Shoulder shrugging
- Arm or hand movement
- Abdomen and pelvic movement
- Bending or gyrating complex movements
- Phonic tics (shouting, screaming, coughing, clucking, swearing and spitting).
Co–morbid conditions patients may have:
- They all have severe TMD
- They are nearly always over–closed with a deep bite
- The condyles are distalised
- They have an under developed maxilla
- Most have Miserable Malalignment Syndrome.
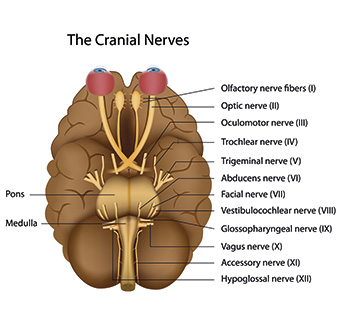
Put simply, the view is that Tourette’s syndrome is caused by compression of the auriculo–temporal nerve by the mandibular condyle; via the trigeminal nerve (V), the effect goes through the subnucleus candalis, which affects the reticular formation, causing crossfiring of inter–neurone connections, which then affect other cranial nerves. The other affected nerves are the facial nerve (VII) causing facial tics, the glossopharyngeal nerve (IX) causing coughing, the vagus nerve (X) causing vocal sounds and the spinal accessory nerve (XI) which causes shoulder shrugging.
The main characteristics seen in Tourette’s cases are cranial growth completed at age five, in boys the maxilla is completed by age seven, in girls the maxilla is completed by age nine and in both sexes the mandible is completed by age nine. Tourette’s is three to five times more common in males, possibly due to the maxillary cranial growth difference.
Case Study
Patient history
Henry was 15 years old when he was referred to the author for treatment of Tourette’s syndrome, which had started five months previously following a seizure. He had glue ear as a child. Brain scan MRI was normal. Henry was under the care of a neurologist.
Symptoms
Spontaneous severe swearing and utterances, supraorbital headaches, continuous popping vocal sounds, seizures (had a fit five months previous), up to 150 tics or involuntary movements in an hour, eye tics (wants to shut his eyes – blepharospasm), head and neck stretching, head banging and punching himself in the head, reduced hearing by 20 per cent and tinnitus in the right ear.
Examination
- Posture: head tilt to the right and rotated to the left, left cranial side bend, dropped right shoulder, dropped instep on the left foot, left knee toed out, pelvis up on the left by 1.5 centimetres, enlarged left trapezius.
- Dental: cross bite on the left, significant clicking in the right TMJ.
- Kinesiology: approximately three times stronger in an edge–to–edge bite.
- TMJ palpation: clicking on the left TMJ.
- Jaw vibrational analysis: right side mid–opening and mid–closing click.
- Electromyography: left temporalis constantly firing at rest. When clenching, the left temporalis was firing three times more than the right.
- Matscan (foot scanner) unstable stance with increased sway, unsteady gait, rotating to the left.
- T–Scan (bite scanner): centre of force back and on right molars.
- Questionnaire results: pain and headaches increased with blepharaspasm and exercise. Sight recently deteriorated significantly over six months from long–sighted to severe short–sighted. Has seen eight specialists for Tourette’s. Patient hears voices in his head saying his name.
- TMJ X–ray: left side (closed) – condyle superiorly and posteriorly displaced. No joint space seen, condylar head flattening with beaking and condylar neck bending. When open, no joint space. Right side – condyle superior displaced and posterior displaced with some joint space.
- Orthotics: patient was wearing foot orthotics, but still the pelvis was up by two centimetres on the left. Head tilt to the right and shoulder dropped on the right. Referred to the podiatrist for new orthotics to ensure pelvis is parallel to the floor.
- Dental findings: significantly micro–dontic with upper cross bite with lower left laterals and canine, Class 1, normal overbite and overjet, narrow airway and large tonsils.
- Masticatory muscle test: all tender, especially the medial and lateral pterygoids and the sternocleidomastoids.
- Range of motion: maximum opening 44mm, left excursion 5mm, right excursion 4mm. Deviation on opening.
- Cervical range of motion: left side bending of head restricted.
- Cranial rhythm: very weak, stronger on the right than left and oscillating. MRI: brain – nothing abnormal detected.
- TMJ: right side Wilkes Classification IV–V. Anterior non–reducing discs with condyle and eminence degeneration and synovitis. Left side Wilkes Classification III–IV. Anteriomedially dislocated disc with reduction on opening. Mild degenerative changes of the condyle and eminence.
- Orthodontic assessment: full photos, lateral skull and OPG, Bimler tracing and study models.
- Orthodontic diagnosis: skeletal class III, Div 2, open bite, dental class II, Div 3. Neutral bite, tongue thrust; factor 1 (position of premaxilla) is minus five degrees.
Treatment proposal
- Upper r–n sagittal appliance to develop the arch.
- Lower TMD splint to reduce the TMD (Tourette’s) and retract the lower incisors.
- Fixed braces to level and align the teeth.
- Veneers on upper 2s
- Retainers
- Estimated treatment time: three years.
Treatment
Henry started his treatment for Tourette’s on 17 February 2011. He was fitted with an upper R–N sagittal appliance and a lower TMD splint to provide him with a more balanced mandibular position.
His inter–incisal opening at this visit was recorded as 44mm. At his second treatment visit two months later, his opening had improved to 51mm. He was now off all his medication and his tics had mainly worsened, except for his eye tics which had reduced considerably. Muscle testing indicated the vertical dimension of the lower splint was correct.
A month later, the patient was much calmer since coming off the medication. Audiology tests noted his hearing was now normal having been 20 per cent down previously. Dramatic improvement in his symptoms with no expletives and only one minor tic occasionally. Opening increased to 54mm.
At this visit, Henry was filmed by ITV for an episode of the documentary “My Child is not Perfect”. In June 2011, Henry reported only occasional tics when stressed; opening now 56mm. He was then referred to the podiatrist for a review of his orthotics.
In July 2011, the upper fixed appliance was fitted and the R–N sagittal was discontinued. The lower splint was being worn full time.
In August 2011, Henry was being treated by a cranial osteopath; orthotics were under construction to level his pelvis. Only one tic seen in the waiting room and one tic in the surgery.
In October 2011, Henry’s neurologist expressed an interest in his dental treatment. Appliances were checked and adjusted.
Between November 2011 and August 2014, Henry’s orthodontic treatment continued with a consistent and apparently permanent improvement in his Tourette’s symptoms, in spite of suffering a severe physical assault while cycling in July 2013. Two months earlier, he passed his driving test.
Now symptom–free, final occlusal corrections were completed and retainers fitted in September 2014. At a three–month follow–up, Henry was symptom–free.
About the author
Dr André Hedger qualified from Guy’s Hospital in London in 1978 (GDC No. 52634). He holds a Bachelor in Dental Surgery and subsequently Licenciate in Dental Surgery degrees. He started his practice in Great Bookham in 1981. He is a fellow of the Hypnotherapy Society and a founder member of the British Society for the Study of Craniomandibular Disorders. André is also a member of the British Orthodontic Society and the International Association for Orthodontics. He is a member of the British Dental Acupuncture Society, the British Society for Clinical and Applied Hypnosis dental phobia certified, the American Academy of Craniofacial Pain, the International Academy of Oral Medicine and Toxicology and Patients Against Mercury Amalgams. He is in the British Society for Dental Sleep Medicine as well as several other specialist groups.