Dentistry’s white-collar crime
In his second article on dental provider fraud, Dr Liam Lynch looks at the reasons dentists commit fraud and what can be done to counter it
In the previous article, the salient issues in Dental Provider Fraud (DPF) were described. In this article, the motivations for DPF are discussed. Some methods of countering this type of fraud are also considered.
Why do dentists engage in DPF?
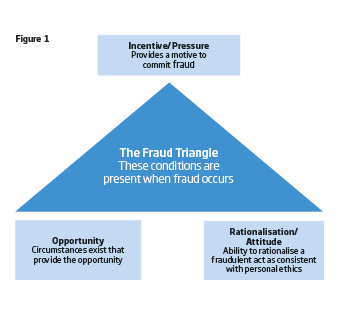
Three factors are hypothesised by Ramos1, to influence whether an individual engages in fraud. These are rationalisation, opportunity and pressure. This hypothesis is described graphically in the well-known Fraud Triangle in Figure 1.
Duffield and Grabosky2 discuss what they term the “psychological factors in fraud”.
They state that at first glance: “A psychological explanation for fraud would appear simple – greed and dishonesty. Such an explanation is, however, overly simplistic. There are many in society who are aggressively acquisitive, but generally law abiding. Moreover, they are also associated with entirely legitimate forms of human endeavour. Technologies of prediction remain imperfect. Not all dishonest people commit fraud. To date, behavioural scientists have been unable to identify a psychological characteristic that serves as a valid and reliable marker of the propensity of an individual to commit fraud.”
When discussing motivation Stotland3 points out that: “…sometimes individuals’ motivation for crime may have originally been relative deprivation, greed, threat to continued goal attainment and so forth. However, as they found themselves successful at this crime, they began to gain some secondary delight in the knowledge that they are fooling the world, that they are showing their superiority to others.”
There is also the gratification obtained from the mastery of a situation. He terms this motivation “ego challenge”.
In 1940, Edwin Sutherland4 coined the phrase “white-collar crime”. Sutherland’s concept of white-collar crime had a ground-breaking polemical impact. Sutherland discredited widely held theories of his day that attributed criminal behaviours to poverty and its associated pathologies.
Sutherland described the white-collar criminal as one who is “respected”, “socially accepted and approved” and “looked up to”.
He later refined his definition of white-collar crime to “crime committed by a person of respectability and high social status in the course of his occupation”5. Fraud committed by dentists in the course of their profession is a perfect example of white-collar crime.
As well as positive motivations for white-collar crimes such as fraud, there are also “weak restraints” that lessen the inhibitions to commit these crimes. In most types of fraud, a majority of offenders may seek to justify or rationalise their activity as hypothesised in the fraud triangle.
In doing so, they will use vocabularies of extenuation6 that manufacture rationale and extenuating circumstances and remove the perception of criminality from the act. For example, frauds against large organisations i.e. insurance companies are often rationalised with the excuse “they can well afford it”.
Another example of neutralisation might include viewing the oral healthcare delivery system as culpable in some respect by not paying an adequate professional fee. Still another is the perception that everyone engages in DPF as part of astute professional practice. In this way, those individual dentists who do not participate are seen as naïve.
Stotland states that white-collar criminals appear to be motivated by money, avoidance of threats to goal attainment, sense of superiority, mastery, the admiration of others and conformity pressures. Psychological restraints on their criminal behaviour are weakened by their jungle view of society, the perception of the moral ambiguity of white-collar crime, the lightness of punishment, the view of victims as being morally culpable, and a belief in their own beneficence.
Stotland concludes that fraud is more likely when remuneration is made from a distant anonymous payment agency rather than from an individual patient.
Countering DPF
Professional fraud in medicine has received considerable attention in the literature, for example Whiting7, Feldman8, and Faunce, Urbas and Skillen9. There was an awareness of the existence of this type of crime by medical practitioners, including dentists, before Sutherland.
A body of literature, perhaps not overly extensive, exists on professional fraud carried out specifically by dentists, for example Pontell, Jesilow and Geis10, Schanschieff, Shovelton, and Toulmin11, Bloomfield12, Welie, 2004b13 and Steele14. A typology of this type of crime was produced by Rocke15.
A conceptual model, developed from the literature, suggests the presence of eight distinct thematic dimensions in countering fraud. These are presented in Figure 2.
Using this model as a framework, we make eight suggestions that may help to counter DPF.
1. As part of developing a counter-fraud culture, and to emphasise the criminality involved, we should use the term fraud rather than the softer euphemisms such as scamming, milking the system or playing the system.
2. As a deterrent, a robust system of pre-enrolment verification, ensuring that the dentist is familiar with the rules and regulations and the terms and conditions of the delivery system, should be in operation.
3. To prevent fraud, a proportion of payments to dentists should be manually checked before payment in an automatic payment system.
4. As an aid to detection, patients should be randomly selected for a clinical peer review examination.
5. As part of the investigation process, failure of the dentist to produce a patient record on request should be routinely followed through.
6. Sanction: all possible sanctions – regulatory, civil and criminal – should be considered in cases of DPF.
7. Redress: the delivery system should have a clear written policy on the recovery of losses incurred to DPF.
8. Monitoring the counter fraud system: the delivery system should regularly review the effectiveness of its counter fraud work against agreed performance indicators.
About the author
Liam Lynch BDS MDPH PhD is a dentist practising in Cork City, Ireland. He has more than 32 years’ experience of active involvement in publicly-funded dentistry. He lectures on the topic of healthcare fraud to MSc students in Healthcare Law and Ethics at the Royal College of Surgeons of Ireland in Dublin. He has published and lectured internationally on probity assurance systems in oral healthcare. In 2013, he was awarded a PhD from The National University of Ireland for his thesis The Counter Practitioner Fraud in Publicly Funded Dentistry Index – A New Dental Instrument. His new book Occupational Fraud in Publicly Funded Dentistry – The Elephant in the Room addresses the main issues in countering this type of fraud. The book was launched at the European Healthcare Fraud and Corruption Network conference in Athens in 2014.
References
1. Ramos M. Auditors’ responsibility for fraud detection. Journal of Accountancy. 2003. [online]. Available at:
www.journalofaccountancy.com/Issues/2003/Jan/AuditorsResponsibilityForFraudDetection jofa/jan2003/ramos.htm
[Accessed:23 March 2015].
2. Duffield G and Grabosky P. The Psychology of Fraud. Crime and criminal justice trends and issues. Canberra: Australian Institute of Criminology, 2001.
3. Stotland E. White collar criminals. Journal of Social Issues 1977; 33(4): 179-196.
4. Sutherland E. White-Collar Criminality. American Sociological Review 1940; 5(1): 1-12.
5. Sutherland E. White Collar Crime. New York: Holt, Rinehart and Winston, 1949.
6. Krambia-Kapardis M. Enhancing the Auditor’s Fraud Detection Ability: An Interdisciplinary Approach. Frankfurt am Main: Peter Lang, 2001.
7. Whiting AD. The Professional Organizations, Training and Ethical Codes of Physicians, Dentists, Nurses and Pharmacists. Annals of the American Academy of Political and Social Science, 1922; 101: 51-67.
8. Feldman R. An Economic Explanation for Fraud and Abuse in Public Medical Care Programs. The Journal of Legal Studies 2001; 30(2): 569-577.
9. Faunce TA. Urbas G. and Lesley Skillen L. (2011). Implementing US-style anti-fraud laws in the Australian pharmaceutical and health care industries. The Medical journal of Australia 2011; 194(9): 474-478.
10. Pontell H, Jesilow P and Geis G. Policing Physicians: Practitioner Fraud and Abuse
in a Government Medical Program. Social Problems 1982; 30(1): 117-125.
11. Schanschieff SG, Shovelton DS and Toulmin JK. Report of the Committee of Enquiry into Unnecessary Dental Treatment. London: Department of Health and Social Security, 1986.
12. Bloomfield K. Fundamental Review of Dental Remuneration. London: Her Majesty’s Stationary Office, 1992.
13. Welie J. Is Dentistry a Profession? Part 2. The Hallmarks of Professionalism. Journal of the Canadian Dental Association 2004; 70(9): 599-602.
14. Steele J. An independent review of NHS dental services in England. London: Department of Health,2009.
15. Rocke S. The War on Fraud and its Effect on Dentistry. Journal of the American Dental Association 2000; 1(131): 241-245.